|
ULTRASOUND IN
TRACHEO-ESOPHAGEAL FISTULA |
- Polyhydramnios.
- The severity and progression of the polyhydramnios is very variable.
- Present in about 90% of cases.
- Rarely develops prior to 24 weeks of gestation.
- Oligohydramnios.
- Can rarely occur in cases of tracheo-esophageal fistula that is complicated by co-existing fetal asphyxia, renal abnormalities or premature rupture of membranes.
- Fetal Stomach.
- Failure to visualize
a fluid-filled stomach. Some fluid is always present in the stomach of a
normal fetus. The stomach does empty periodically and may not be seen for
brief periods (<30 minutes).
Failure to refill in a 30 minute period is suggestive of some obstruction to swallowing.
The combination of polyhydramnios and failure to visualize the fetal stomach is virtually diagnostic. - A small rim of fluid may be present in the stomach from either tracheal fluid passing into the stomach from the fistulous tract or from normal gastric secretions.
- The probability of obtaining a correct diagnosis is only 42% on the basis of polyhydramnios and a stomach that is either absent or shows reduced filling (1). The most reliable predictor is the presence of a blind ending pouch in the fetal neck or upper mediastinum.
- Pretorius et.al. (9) in a retrospective review reported that:
- Only 7/22 infants born with TEF had both polyhydramnios and no visible stomach.
- In a further 7 pregnancies, polyhydramnios and a fetal stomach were both detected sonographically.
- None of these women developed polyhydramnios prior to 24 weeks.
- 12/22 infants had other anomalies.
|
Proximal esophageal
atresia with a distal tracheo-esophageal fistula |
|
|
|
|
|
|
|
- Visualization of the fluid filled blind upper end of the esophagus is possible in some fetuses. The fetus appears to constantly empty fluid from the blind pouch into the glottis and amniotic cavity.
|
|
|
|
- Swallowing movements are usually present and normal.
- The fetal trachea is inconsistently visualized. To date the fistulous tract between the esophagus and trachea cannot be identified.
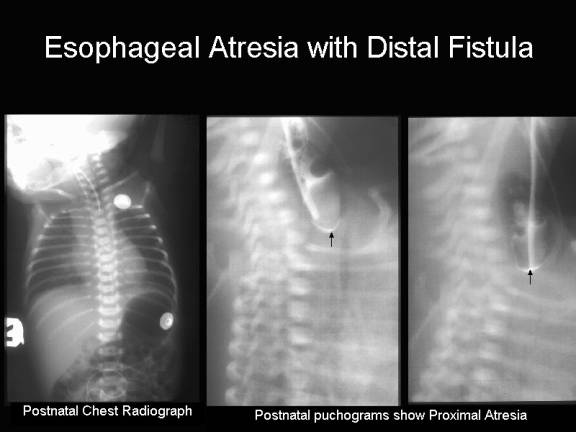
- Esophageal Atresia With Distal Fistula.
|
Esophageal Atresia With Distal Fistula. |
|
|
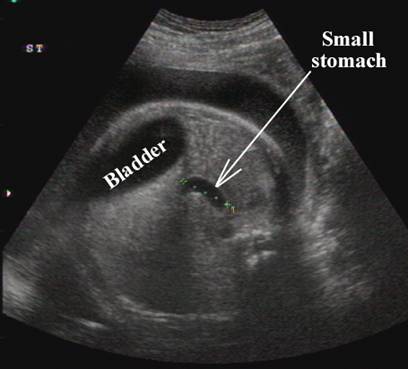
Polyhydramnios |
|
|
|
|
|
Small stomach – fluid in stomach through small
fistula between distal trachea and esophagus |
|
|
|
|
|
Postnatal
radiograph – pouch in fetal neck and air in the stomach and small bowel |
|
|
|
|
|
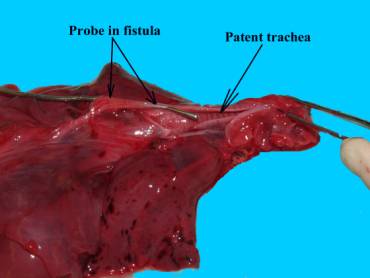
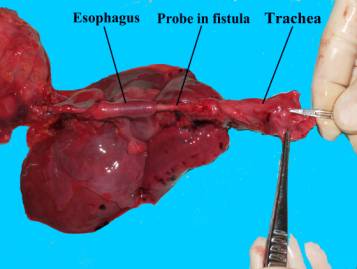
Postnatal pathological specimen in another infant that
died. Note the surgical probe in the fistula between the distal trachea and esophagus |
|
|
|
|
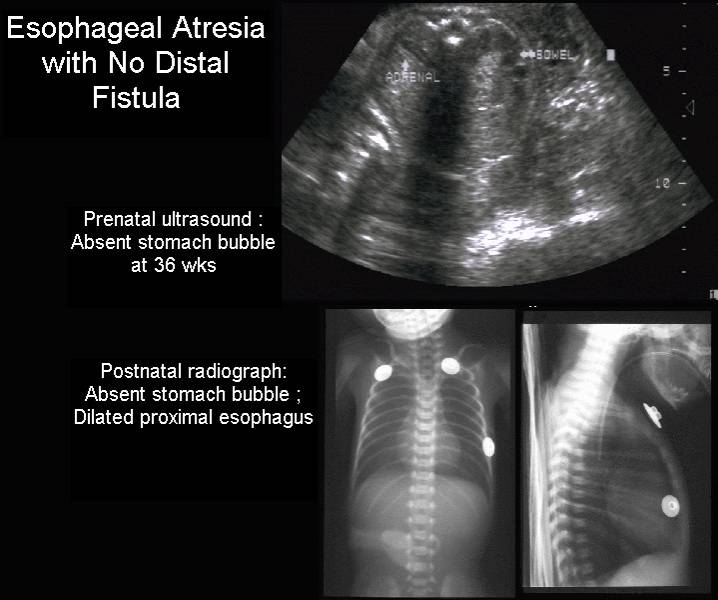
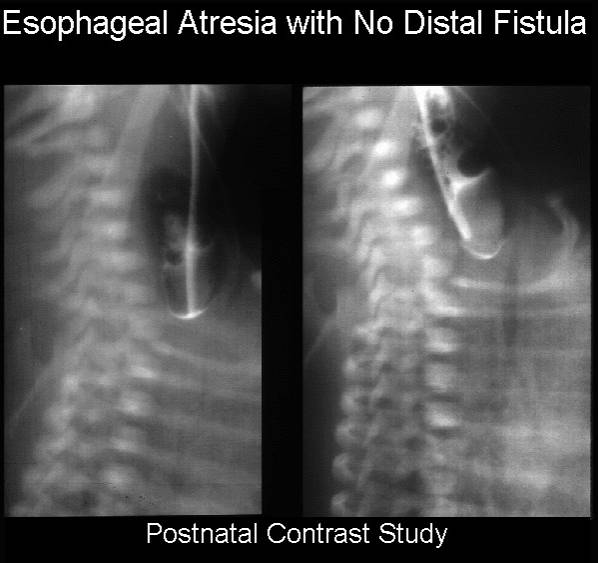
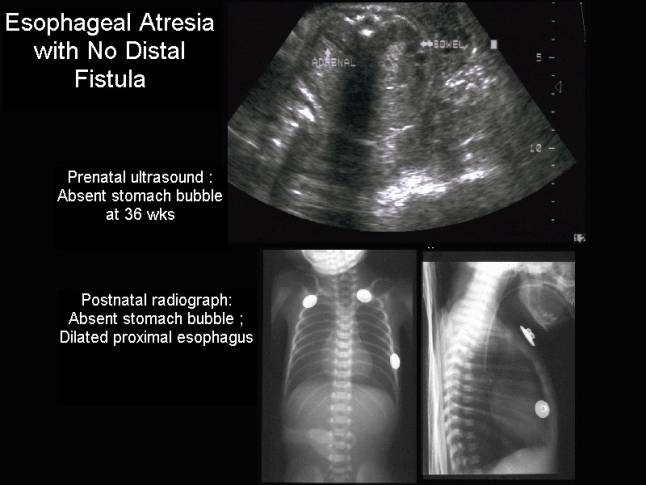
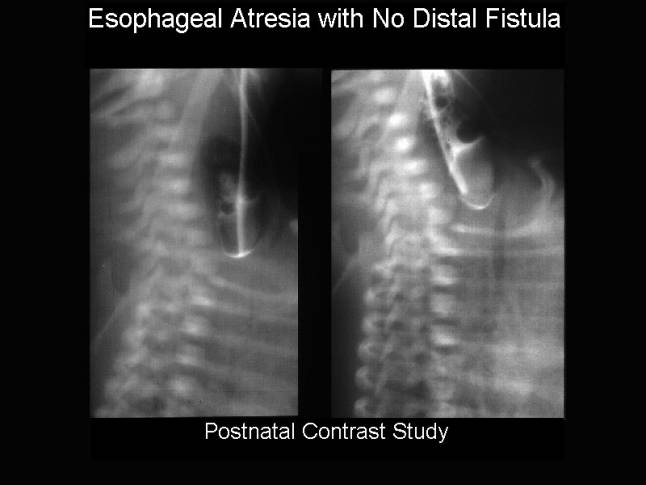
- Esophageal Atresia Without
Distal Fistula.
|
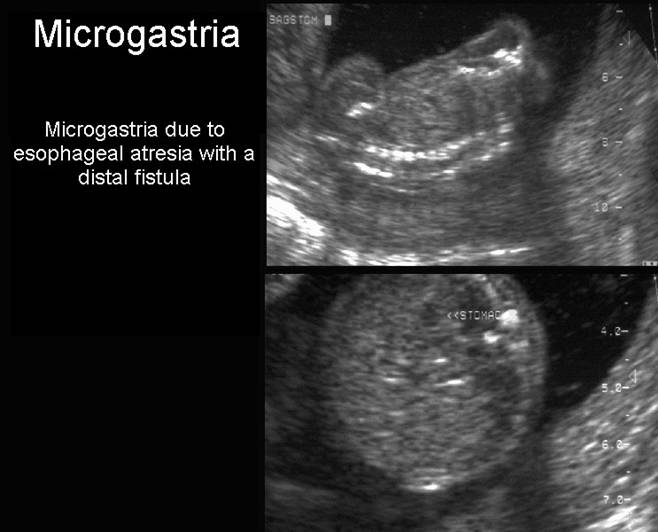
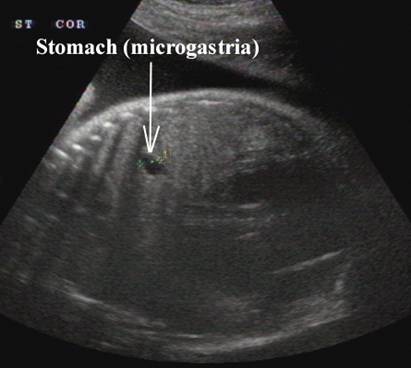
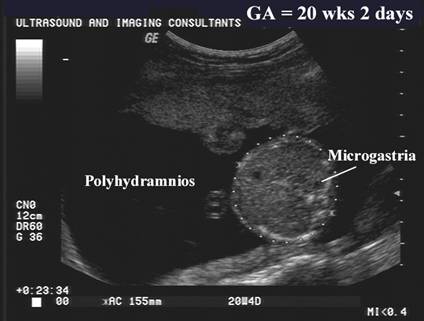
Esophageal
atresia without a distal fistula – ·
Severe microgastria. ·
Absent stomach. ·
Polyhydramnios. |
|
|
|
|
|
|
|
|
|
|
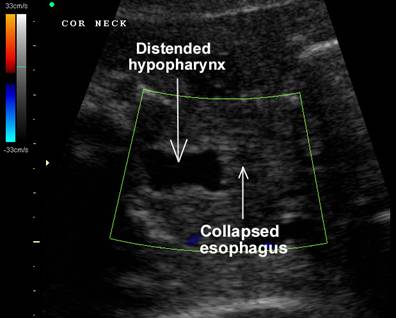
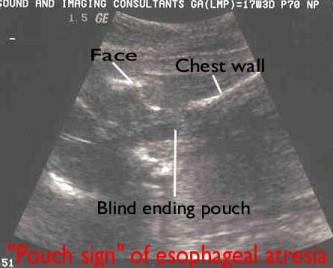
- Visualization of the fluid filled blind upper end of the esophagus is possible in some fetuses "Pouch Sign" (4). The fetus appears to constantly empty fluid from the blind pouch into the glottis and amniotic cavity.
The pouch may be in the cervical region ("neck pouch") or in the upper mediastinum ("mediastinal pouch" – below the clavicles). This differentiation is important with respect to postnatal repair. Pouches with the base situated in the thorax are always associated with a distal tracheo-esophageal fistula and primary esophageal repair is possible. In pouches situated higher, with the base in the neck, primary repair was not possible (1). This is because neck pouches are associated with a longer atretic gap (and a higher probability of severe associated anomalies) (1). Although onset has been observed as early as 23 weeks, and 26 weeks, several reports suggest that it is a late sign (3,7,8). It is thought that in the first and second trimesters of pregnancy the fetus is unable to develop sufficient pressure in swallowing to dilate a blind esophagus (8).
· The probability of obtaining a correct diagnosis is only 42% on the basis of polyhydramnios and a stomach that is either absent or shows reduced filling (1). The most reliable predictor is the presence of a blind ending pouch in the fetal neck or upper mediatinum.
· Visualization of the fluid filled blind upper end of the esophagus is possible in some fetuses "Pouch Sign" (4). The fetus appears to constantly empty fluid from the blind pouch into the glottis and amniotic cavity.
The pouch may be in the cervical region ("neck pouch") or in the upper mediastinum ("mediastinal pouch" – below the clavicles). This differentiation is important with respect to postnatal repair. Pouches with the base situated in the thorax are always associated with a distal tracheoesophageal fistula and primary esophageal repair is possible. In pouches situated higher, with the base in the neck, primary repair was not possible (1). This is because neck pouches are associated with a longer atretic gap (and a higher probability of severe associated anomalies) (1).
|
“Pouch Sign” in two different
fetuses |
|
|
|
|
|
|
|
REFERENCES |
1. Kalache KD, Waumer R, Mau H, Chaoui R, Bollman R. Prognostic significance of the pouch sign in fetuses with prenatally diagnosed esophageal atresia. Am J Obstet Gynecol 2000;182:978-981.
2. Okada,
A, Usui N, Inoue M, Kawahar
H et.al. Esophageal atresia in
3. Stringer MD, Mckenna KM, Goldstein RB et.al. Prenatal diagnosis of esophageal atresia J Pediatr Surg 1995;30:1258-1263.
4. Kalache KD, Chaoui R, Mau H et.al. The upper neck pouch sign: a prenatal sonographic marker for esophageal atresia. Ultrasound Obstet Gynecol 1998;11:138-140.
5. Vijayaraghavan SB. Antenatal diagnosis of esophageal atresia with tracheoesophageal fistula. J Ultrasound Med 1996;15:417-419.
6. Kulkarni B, Rao RS, Oak S, Upadhaya MA. 13 pairs of ribs – a predictor of long gap atresia in tracheoesophageal atresia. J Pediatr Surg 1997;32:1453-1454.
7. Schulman A, Mazkereth R, Zalel Y et.al. Prenatal identification of esophageal atresia: the role of ultrasonography for evaluation of functional anatomy. Prenat Diagn 2002;22:669-674.
8. Centini G, Rosignoli L, Kenanidis A, Petralgia F. Prenatal diagnosis of esophageal atresia with the pouch sign. Ultrasound Obstet Gynecol 2003;21:494-497.
9. Pretorius D, Meier P, Johnson M. Diagnosis of esophageal atresia in utero. J Ultrasound Med 1983;2:465-476.